
The Effect of Sleep on Hypertension and 8 Secrets to A Good Sleep
Share
Hypertension is one of the major causes of cardiovascular diseases and deaths worldwide. Hypertension itself is a complex disease, which is mainly influenced by environmental and genetic factors. Sleep as an important modifiable risk factor for hypertension has also attracted the attention of researchers all over the world.
Today, we’re going to discuss the implications between sleep and hypertension.
Sleep Duration and Hypertension
There is a relationship between sleep duration and risk of hypertension. However, getting too much or too little sleep can increase the risk of high blood pressure.
Studies have shown that the risk of hypertension is minimal when you sleep for 7-8 hours. In 2018, an article published in the Journal of Clinical Sleep Medicine collected data from a total of more than 700,000 people from the 2013 U.S. Behavioral Risk Factor Surveillance System and the 2007-2016 U.S. National Health Interview Questionnaire, to analyze and study the relationship between sleep duration and hypertension【1】.
Figure 1 The implication between sleep duration and hypertension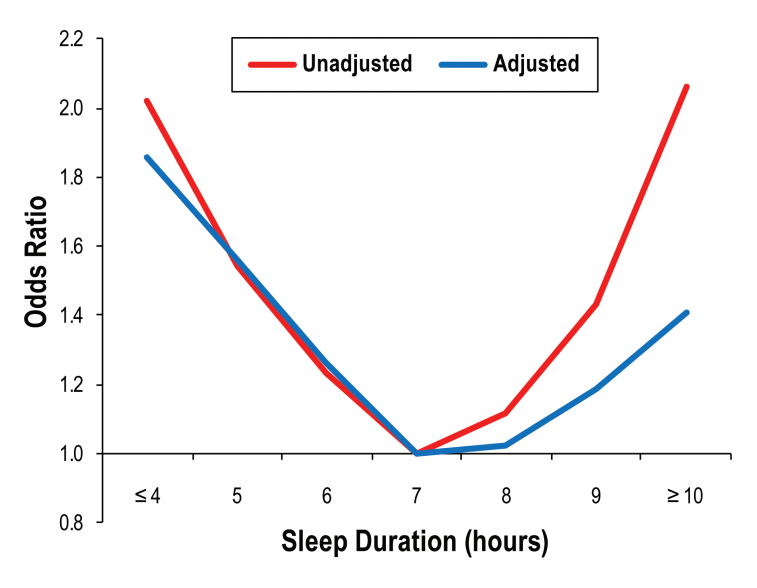
In adjusted analyses, compared to 7 hours, increased risk of hypertension was seen among those sleeping ≤ 4 hours (odds ratio [OR] = 1.86, P < .0005), 5 hours (OR = 1.56, P < .0005), 6 hours (OR = 1.27, P < .0005), 9 hours (OR = 1.19, P < .0005), and ≥ 10 hours (OR = 1.41, P < .0005 (see Figure 1 above). When stratified by age, sex, and race/ethnicity groups, short sleep was associated with increased risk for all age groups < 70 years, and long sleep (≥ 10 hours only) was associated with risk for all except < 24 years and > 74 years.
Obstructive Sleep Apnea and Hypertension
Obstructive sleep apnea (OSA, obstructive sleep apnea) is caused by the collapse of the upper airway during sleep, causing a series of transient suffocation and hypoxemia, brain arousal, sleep problems, and daytime sleepiness, which is one of the risk factors for hypertension. OSA is very common in the hypertensive population (30%-50%), particularly those with resistant hypertension (80%)【2】. OSA, especially moderate-to-severe OSA, is associated with prevalent and incident hypertension. In 2018, a meta-analysis of 26 studies showed that OSA was associated with an approximately 3-fold higher risk of resistant hypertension. Furthermore, mild (apnea-hypopnea index [AHI] >5), moderate (AHI >15) and severe OSA (AHI >30) were associated with an increased risk of hypertension by 18%, 32% and 56%, respectively 【3】.

For healthy individuals, their nighttime blood pressure typically decreases by 10%-20%, which is sometimes referred to “blood pressure dipping”. Those who have severe OSA had less than 10% drop in their nocturnal blood pressure. Researchers reported that people whose blood pressure rises while they're sleeping have a higher risk for cardiovascular disease【4】. In addition, many patients with OSA wake up with a sudden and significant increase in blood pressure in the morning, which would be another factor that may increase the risk of cardiovascular disease. Moderate to severe OSA increases all-cause and cardiovascular mortality.
Therefore, the treatment and improvement of sleep apnea is of great significance for reducing the risks of hypertension and cardiovascular diseases.

How To Get A good Night's Sleep
Here are 8 tips for a good night’s sleep from Harvard Heath:
- Exercise
Don’t use your bed as an office for answering phone calls and responding to emails. Avoid watching late-night TV in bed. Beds are supposed to stimulate sleep, not for wakefulness.
- Keep it comfortable
When we were kids, our parents probably told us bedtime stories. A sleep ritual that helps us develop good sleep habits and make it easier to fall asleep. Even for adults, a bedtime ritual can have a similar effect. Sleep rituals help signal the body and mind that it's time to sleep. Drinking a glass of warm milk, taking a bath, or listening to music before bed can all be relaxing as a sleep ritual.

- Eat, but not too much
Too hungry or too full will keep you awake. Avoid large meals within 2-3 hours of bedtime.
- Avoid alcohol and caffeine
Many of us know that both alcohol and caffeine can be a stimulant. They will disrupt sleep during the night. You would also need to stay away from anything acidic (such as citrus fruits and juices) or spicy, which can give you heartburn and make it difficult for you to fall asleep.
-
De-stress
Daytime worries can bubble to the surface at night. Stress is a stimulus that distracts your sleep. Give yourself time to wind down before bed. Try to learn some form of the relaxation response can help you sleep well and reduce daytime anxiety.
- Get checked
Restless legs syndrome, sleep apnea, and gastroesophageal reflux are three common sleep disrupters. If there symptoms are keeping you up at night or making you sleepy during the day, you need to get helps from your doctor.
